You are a Physician
Aesthetic doctor, plastic surgeon,
cosmetic dermatologist
You are a Company
Pharmaceutical, Biotech,
Medical Device
Our solutions and services
All-in-one solution for your consultation needs
Photo standardizing is a challenge faced by aesthetic practitioners.
Bridge this gap by integrating our all-in-one 3D cameras into your practice. Capture face, body and breast images for easy and accurate patient follow-up.
Management and evaluation of clinical trials photography
Proving the efficacy and safety of treatments is fundamental in clinical trials.
QuantifiCare provides the standardization and real-time monitoring you require by using our imaging services tailored to your specific approach.
Years experience
Countries
innovation Awards
We are global
QuantifiCare operates globally while providing flexibility, knowledge and support locally.
We have offices in the USA, France, Brazil and the Philippines and distribution partners covering over 50 countries around the world.
They trust us
 QuantifiCare’s LifeViz® Infinity technology, allows us to record the details of each individual’s beauty.
QuantifiCare’s LifeViz® Infinity technology, allows us to record the details of each individual’s beauty.
We are in the heart of the Amazon, a region well-known in the world for the wealth of its natural resources, where the people have on their skin the characteristics of a mixing as vast as Brazil itself.
I am very happy to be able to offer state-of-the-art technology to patients; we are the first clinic in Latin America to have 2 sets of QuantifiCare’s LifeViz® Infinity technology, which allows us to record the details of each individual’s beauty and track the progress of their treatment through a feature only found in the best clinics in the world.
Dr. Adriana Mariano, Dermatologist, Brazil
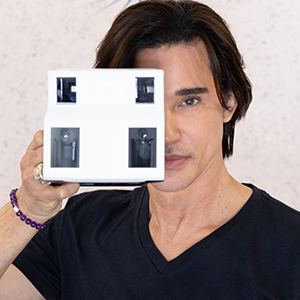 LifeViz® Mini Pro is the best choice for me, my practice and my patients.
LifeViz® Mini Pro is the best choice for me, my practice and my patients.
I feel that QuantifiCare has a real talent for building on their expertise and innovation.
The LifeViz® Mini Classic has been an invaluable addition to my practice, but I am ready to upgrade to the LifeViz® Mini Pro as I want to provide the very latest technology for my patients.
It’s what they expect. I can have a premium, effective, simple and cutting-edge solution that will really make a difference to my consultations.
Dr Shino Bay, Aesthetic Dermatologist, USA
 The LifeViz® Mini is an extremely good system that simplifies evaluation and elevates your clinic to a higher level scientifically
The LifeViz® Mini is an extremely good system that simplifies evaluation and elevates your clinic to a higher level scientifically
My name is Thomas Rappl, I’m a plastic surgeon from Graz in Austria, and I’m also an IMCAS scientific secretary.
Why do I use the LifeViz® Mini?
I find the camera system extremely good. First, because it’s easy and simple to understand and to use. The second reason is that I need it for my presentations. The presentations just become significantly more scientific and more perfect. Everything that has been done is clear and can be evaluated. The last reason is that it is also important for the patients, when they come to the clinic to take a photo before and after the treatment. One photo can really demonstrate how much is changing during the treatment, whether it be with toxins, fillers or EBD devices, like micro focused ultrasound or whichever treatment is chosen.
The LifeViz® Mini is an extremely good system, that simplifies evaluation and elevates your clinic to a higher level scientifically. I can therefore only recommend it and hope you enjoy using it.
Dr Thomas Rappl, Plastic Surgeon, Austria
Events
- MIA, Sao Paulo, 16 - 18th Nov 23
- PSTM, Boston, 27 - 30th Oct 23
- BOT, Sao Paulo, 20 - 22th Oct 23
- GAC, Miami, 19 - 22th Oct 23
- CONGREHOF, Brazil, SC, 05 - 07th Oct 23
- Meidam, Dubai, 22 - 24th Sep 23
- SFME, Paris, 15 - 16th Sep 23
- CSBD, Florianópolis, 07 - 09th Sep 23
- SSDV, Lausanne, 06 - 08th Sep 23
- CICPGRJ, Rio de Janeiro, 17 - 19th Aug 23
- MAC, San Diego, 02 - 05th Aug 23
- IMCAS Amercias, Cartagena, 20 - 22th Jul 23
- TAS, Las Vegas, 06 - 09th Jul 23
- WCD, Singapore, 03 - 08th Jul 23
- FACE, London, 30 - 01st Jun Jul 23
- PEM Cosmiatria, Sao Paulo, 25 - 27th Jun 23
- AMWC Brazil, Sao Paulo, 22 - 24th Jun 23
- BTS, Stockholm, 01 - 03th Jun 23
- RADLA, Brazil, PR, 27 - 30th May 23
- AECD, Sao Paulo, 25 - 27th May 23
- SCALE, Nashville, 17 - 21th May 23
- Nice Tox, Nice, 12 - 13th May 23
- DDL, Berchtesgarden, 04 - 07th May 23
- CBCD, Rio de Janeiro, 20 - 23th Apr 23
- ASLMS, Phoenix, 13 - 16th Apr 23
- AMWC, Monaco, 30 - 01st Mar Apr 23
- Derm, Frankenthal, 24 - 26th Mar 23
- LAMCA, Beverly Hills, 23 - 26th Mar 23
- Shino Bay World Tour, Sao Paulo, 18 - 19th Mar 25
- FACE Salvador, Salvador, 15 - 17th Mar 23
- Dubai Derma, Dubai, 01 - 03th Mar 23
- AMWC NA, Miami Beach, 23 - 25th Feb 23
- IMCAS, Paris, 28 - 30th Jan 23
- CIOSP, Sao Paulo, 25 - 28th Jan 23